Coxarthrosis is a disease that affects a patient's hip joint. The treatment is long-term. A few decades ago, such a diagnosis was practically a sentence for a patient who promised him: severe exhausting pain, a gradual decrease in mobility, early disability.
But thanks to the most effective modern treatment methods, it has become possible not only to stop the degenerative process, but also to completely cure coxarthrosis in the early stages.
Understanding the causes of the disease has raised the issue of an integrated approach to therapy. Treatment of hip arthrosis may include medication and physiotherapy.
What is hip arthrosis
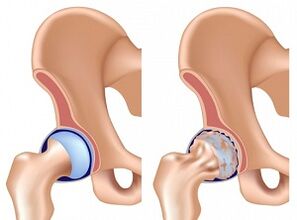
Arthrosis is a disease in which the normal structure of cartilage in the joints is disrupted. Unlike arthritis, deformity is not caused by infectious tissue inflammation but by a violation of metabolic processes.
Deforming hip arthrosis, with rare exceptions, can be observed in patients over 40 years of age. The development of the pathology is as follows:
- Metabolic disorder. Cartilage has no blood vessels, so it nourishes the adjacent muscle tissue. The synthesis of substances is interrupted for various reasons.
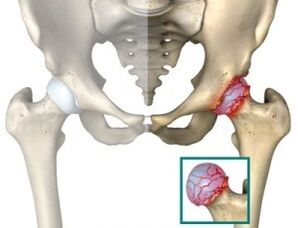
- Cartilage starts to lose its elasticity due to insufficient nutrition. It becomes thinner over time. The interosseous lumen is significantly reduced. Grade 3 hip arthrosis is characterized by the fact that bone tissue growths rub against each other. Cartilage is virtually absent.
- Bone loading, which reduces cartilage thickness, contributes to bone deformity.
After the onset of degenerative changes, it can take years for the patient to develop in the third stage of the disease, but under adverse conditions and if precautions are not taken, pathological changes can occur much more quickly.
How arthrosis manifests itself
The symptoms and nature of hip arthrosis depend on the extent of the disease. The most common symptom is pain. Patients most often seek medical help for pain due to pain. In addition, the insidiousness of the disease is that in the early stages of degenerative changes, pain usually does not cause great discomfort, is short-term in nature, and is often attributable to normal fatigue.
Thedelay results in the missed moment of starting treatment and requires more time and effort to cure grade 2 hip arthrosis. The chances of a successful prognosis remain, provided the therapy is prescribed correctly.
The symptoms of the disease are as follows:
- Pain - may occur in the thigh, groin and the joint itself. You should be careful if your pain symptoms are at rest. This indicates the urgent need to visit an arthrologist.
- Stiffness of movement, limping. It can be observed after prolonged immobility of the foot, such as after sleep.
- Over time, the patient’s feet will become shorter than the healthy, muscle tissue atrophy observed that is felt.
Modern diagnostic tests cannot be dispensed with when diagnosing a disease. Thus, grade 1 hip arthrosis is diagnosed only by X-ray, CT, and MRI. The changes and narrowing of the interosseous lumen are clearly visible in the image.
Stages of hip arthrosis
Once the pathology is diagnosed, the patient is assigned a code according to ICD 10. This is an international classification of diseases that is reviewed every 10 years.
Thanks to the assigned code, we don't just collect statistics. Therapies can be selected that produce the most tangible results. Thanks to international collaboration, medical treatment for hip arthrosis has improved significantly over time.
World practice has recognized that there are three stages or stages of development of hip arthrosis. Each of them has its own symptoms. Namely:
- First section.The feeling of pain only occurs in the background of overwork: running, exercise, exercise, etc. The pain is mainly concentrated in the joint area. The pain usually goes away on its own after some rest. In this case, the mobility of the leg remains complete, muscle strength is not limited. Grade 1 arthrosis can only be diagnosed by X-ray or tomography. The picture clearly shows small deformations of the bone tissue that do not extend beyond the so-called joint lip. The joint gap narrows slightly, usually in uneven areas.
- Second section.It is characterized by migratory pains that begin to spread to the groin, thigh. May occur spontaneously during rest. The pain in hip arthrosis in the second stage does not go away on its own and the patient needs anesthesia. The range of motion is disturbed, muscle tissue atrophy is observed. The picture shows the bone growths and deformities of the femoral head. Perhaps the appearance of a cyst on the most stressed part of the thigh - the acetabulum. The diagnosis of arthrosis in the second stage is made quickly. Abnormal changes are evident even in a superficial examination. X-rays or MRIs are taken to see the degree of deformity.
- Third section.The pain is starting to become chronic. Arthrosis can be determined without a thorough examination. The patient cannot move without reeds, the pelvis tilts, leading to shortening of the foot. When moving, the patient should tilt his torso to the injured joint. As a result, this leads to even greater degenerative changes. The image shows extensive bone deformities. The joint gap is almost invisible.
Therapeutic treatment of deforming hip arthrosis is effective only in stages 1-2 of the disease. The third stage of pathological development often necessitates surgical intervention.
How to treat arthritis in the hip joint
Regardless of what you use, gymnastics for hip arthrosis or medication, each approach is based on six principles. Namely:
- Take off the pain.
- Provide normal cartilage tissue nutrition and restore if possible.
- Improve blood flow to the affected area.
- Reduce joint stress.
- Strengthen the atrophic muscles.
- Replace joint mobility.
Complex therapy must be used to achieve all six goals. So, for example, injections can be given into the joint, but without ensuring that the load is reduced, all the beneficial effects of chondroprotectors can be destroyed. Unsurprisingly, in world practice, 2-10 different approaches are usually used simultaneously, depending on the patient’s condition.
How to treat hip arthrosis

A comprehensive approach to hip treatment provides better results than a single therapeutic agent - this has been recognized by the world’s leading arthologists. Therefore, it is not uncommon for a patient to be prescribed multiple treatments at once from the following:
- NSAIDs- non-steroidal anti-inflammatory drugs are the "classics" of treatment. Medicines for arthritis of the hip joint should be prescribed either in combination with non-steroidal drugs or in their composition. NSAIDs are particularly effective in exacerbating the disease. They help relieve pain and reduce swelling. The reception allows you to practice hip arthrosis, massages, gymnastics and other physiotherapy procedures. The disadvantage of NSAIDs is their negative effect on the gastric mucosa. Patients need to understand that non-steroidal drugs for hip arthrosis do not cure the disease but simply eliminate the symptoms, allowing therapy.
- Chondroprotectors and hyaluronic acid.These drugs are a new stage in the treatment of the hip joint and can therefore be classified into a separate group.
- Chondroprotectors are prescribed as restorative therapy. With prolonged use, chondroprotectors repair damaged cartilage tissue, but their effectiveness is limited by the initial stage of the disease.
- Hyaluronic acid builds up a layer between the bones, so less stress can be achieved on the joint. Effective as restorative therapy.
- Muscle relaxants- vasodilators that can relieve muscle cramps. It is prescribed to reduce the load on the joint. Muscle relaxants should only be used as part of a complex medication.
- Anesthetic Ointment- Despite advertisements for ointments as a panacea for relieving the disease, they actually only eliminate the unpleasant symptoms of the disease. On the other hand, analgesics in the form of ointments enhance the effectiveness of conservative treatment, allowing relief of swelling and alleviation of the patient's condition.
- Intra-articular injections- to relieve pain, repair cartilage or protect against excessive pressure on the joint. The most commonly used drugs are corticosteroids. They relieve the pain by allowing the patient to start treatment with physical therapy. Hyaluronic acid preparations may also belong to the group of corticosteroids. The effectiveness of intraarticular injections depends largely on how experienced the surgeon is (statistics show that 30% of doctors miss the joint capsule when they perform manipulations).
Some medicines can be harmful to your body. Self-healing is strictly forbidden!
Hip joints relieve joint stress and reduce the factor that is a major cause of tissue irritation leading to the inflammatory process. Therefore, in conjunction with drug therapy, fixation of the injured area is often required.
Alternative Methods and Physiotherapy
In addition to prescribing anti-inflammatory drugs, intraarticular injections, and other medications, the patient may undergo physiotherapy and use non-traditional therapies.
- Manual Therapy- This procedure has a softer effect on damaged tissues than massaging the hip joint in case of arthrosis. Any aggressive effect on the injured area can easily trigger the onset of the inflammatory process. Manual therapy is not yet common in our field, but it is widespread in the West and is one of the official methods of therapy.
- Physiotherapy for deforming arthrosisis a huge area where the patient can choose between traditional and non-traditional methods. Pilates, yoga, as well as water exercises and other ways to restore atrophic muscle function with hip arthritis are popular. Physical education and moderate effort, along with medications, have a beneficial effect and contribute to the patient’s recovery.
- Traditional Medicine- Most arthrologists oppose this method as a stand-alone therapy. And their opinion has a basis. The majority of patients, rejecting the help of traditional medicine, acquired a disability for themselves. But under the supervision of a treating physician, effective treatment of hip arthrosis with folk remedies is entirely possible. Most of the herbs and infusions used have anti-inflammatory and analgesic effects. Some medication costs have serious contraindications, so consult an arthologist before use. We recommend that you use unusual alternative methods to treat hip arthrosis with caution. Some recipes not only do not contribute to improvement, but also lead to the opposite effect, causing accelerated cartilage destruction.
- Homeopathy- helps to normalize the synthesis of substances in the body. Homeopathy is especially effective in post-traumatic arthrosis, which allows it to cope with the main factor that led to the development of the disease.
- Apitherapy- treatment with bee bites is very effective, it allows to combine acupuncture and medication. Not surprisingly, many warming and effective ointments contain processed bee venom. Apitherapy is often more effective than hip blocking. The appropriateness of using apitherapy should be decided by the treating physician.
- Magnetotherapy- is used to supplement the treatment and prevention of the disease. The effect of the magnet increases the blood flow of the tissues, helps to restore metabolic processes. Removes salt.
- Hirudotherapy- Leech therapy has been used for centuries. Leech saliva, which enters the bloodstream, has been shown to contain a substance that promotes its liquefaction. As a result, blood can even enter atrophic capillaries and blood vessels.
- Mud Therapy- has a mild warming effect, helps to get the necessary nutrients. Proper application of mud therapy reduces inflammation and pain. Purulent arthrosis of the hip joint is prohibited. It is prescribed with caution in the presence of blood clots and vascular disease.
- Shilajit for arthrosis- used in pure form, as part of tinctures and compresses. The beneficial ingredients that make up Mumiyo promote tissue regeneration. Mumiyo is especially effective in the early stages of the disease.
- Self-massage- sharp aggressive applause and pressure are ruled out. Blood and lymph flow must be ensured during massage. A chiropractor or an experienced massage therapist will show you the types and direction of your movements.
Treatment of hip arthrosis at home by non-traditional methods should be supplemented with adequate nutrition.
If you consume only 5 kg, the probability of the onset of the inflammatory process is reduced by about 30%.
Hip arthrosis and pregnancy
Pregnancy with hip arthrosis is a double stress for the female body. Most medications are prohibited during pregnancy. At the very least, great care must be taken not to harm the baby.
If hip arthrosis is in the early stages of pregnancy, medication should be postponed after delivery.
It is possible to give birth with arthrosis in the hip joint, but you need to understand all the risks involved. Complications after childbirth are not uncommon and cartilage tissue deformity is increased.
A full body examination should also be performed when planning the child. All medications, ointments, and painkillers should only be taken as directed by your doctor.
Consequences of arthrosis
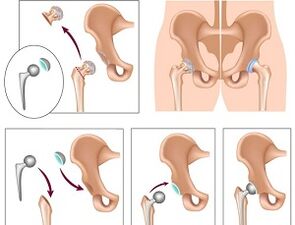
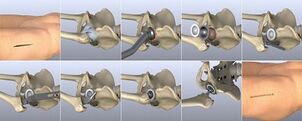
In the late stages of the disease, it becomes impossible to cure coxarthrosis in the usual way. Surgery is needed. The operation is a final solution and can be performed in different ways.
- Joint Replacement- completely restores all motor functions. The disadvantage of this solution is the limited life of the prosthesis. After an average of 15 years, it requires a second operation to replace it.
- Laser therapy for surgical arthrosis of the hip joint- used to reject a joint in the bone. Using laser therapy, the damaged surface is removed and replaced with an artificial insert.
All types of surgical interventions are temporary, but without them the patient becomes disabled.
Early diagnosis of coxarthrosis and properly prescribed restorative therapy are the only reliable ways to combat the disease. Ignoring the symptoms leads to disability.



































